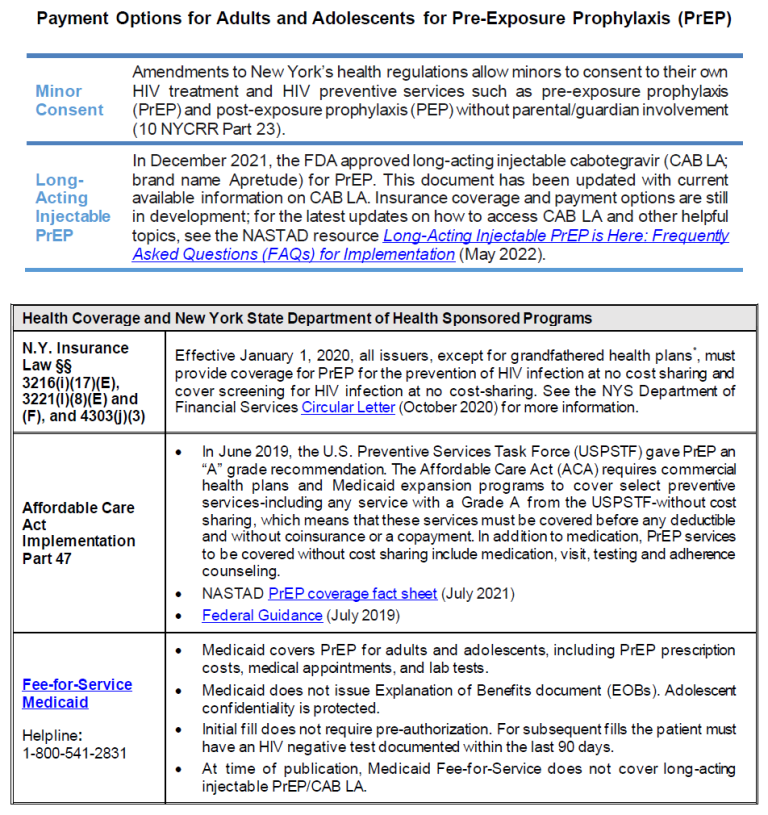
PrEP Payment Options
Guidance for HIV Testing of Sexual Assault Defendants
Download Printable PDF of Guidance for HIV Testing of Sexual Assault Defendants
Reviewed and updated: New York State Department of Health AIDS Institute (NYSDOH AI); January 2024
Purpose of This Guidance
As of November 1, 2007, New York Criminal Procedure Law § 210.16 requires testing of criminal defendants, indicted for certain sex offenses, for HIV, upon the request of the sexual assault survivor.
The NYSDOH is responsible for issuing guidance for the court on the following:
- Medical and psychological benefits to the survivor.
- Appropriate HIV test to be ordered for the defendant.
- Circumstances when follow-up testing for the defendant is recommended.
- Indications for discontinuation of post-exposure prophylaxis (PEP).
The NYSDOH AI’s Medical Care Criteria Committee (MCCC) and the Mental Health Guidelines Committee carefully reviewed the issues involved and developed this guidance in 2007 through a consensus-based process, and updated it as needed, most recently in January 2024. As requested, the Committee specifically addressed HIV risk; however, care providers should also consider the risk of transmission of hepatitis B, hepatitis C, and other sexually transmitted infections in any sexual assault patient. The guideline PEP to Prevent HIV Infection, developed by the MCCC of the NYSDOH AI, includes recommendations for the post-exposure management of HIV, hepatitis B virus, and hepatitis C virus in sexual assault patients.
Definitions of Significant Risk of HIV Through Sexual Assault Exposure
The defendant testing law refers to “significant exposure” as defined by 10 NYCRR § 63.10. The NYSDOH AI guideline PEP to Prevent HIV Infection offers a definition of significant exposure during sexual assault that warrants assessment of the survivor. Both definitions are listed below.
- “Significant risk” as defined by 10 NYCRR § 63.10: Three factors are necessary to create a significant risk of contracting or transmitting HIV infection:
- The presence of a significant-risk body substance, and
- A circumstance that constitutes significant risk for transmitting or contracting HIV infection, and
- The presence of an infectious source and a noninfected person.
- Significant risk body substances: Blood, semen, vaginal secretions, breast milk, tissue, and the following body fluids: cerebrospinal, amniotic, peritoneal, synovial, pericardial, and pleural.
- Circumstances that constitute “significant risk of transmitting or contracting HIV infection” for sexual assault survivors:
- Sexual intercourse (e.g., vaginal, anal, oral) that exposes a noninfected individual to blood, semen, or vaginal secretions of an individual with HIV.
- Sharing of needles and other paraphernalia used for preparing and injecting drugs between individuals with and without HIV.
- Penetrating injuries (such as needlesticks with a hollow-bore needle) with exposure to blood or other potentially infected fluids from a source known to have HIV or whose HIV status is unknown.
- Bite from a person known to have HIV or whose HIV status is unknown with visible bleeding in the mouth that causes bleeding in the exposed person.
- Other circumstances not identified during which a significant-risk body substance (other than breast milk) of an individual with HIV contacts mucous membranes (e.g., eyes, nose, mouth), nonintact skin (e.g., open wound, skin with a dermatitis condition, abraded areas), or the vascular system of an individual without HIV.
- Circumstances that do not involve “significant risk”:
- Kissing if no blood is exchanged due to sores or bleeding gums.
- Exposure to urine, feces, sputum, nasal secretions, saliva, sweat, tears, or vomitus that does not contain blood that is visible to the naked eye.
- Human bites where there is no direct blood-to-blood or blood-to-mucous membrane contact.
- Exposure of intact skin to blood or any other bodily substance.
The NYSDOH AI guideline PEP to Prevent HIV Infection defines a significant exposure during “sexual assault” as follows:
- When the exposed individual has experienced direct contact of the vagina, penis, anus, or mouth with the semen, vaginal fluids, or blood of a defendant, with or without physical injury, tissue damage, or presence of blood at the site of the assault.
- When the exposed individual’s broken skin or mucous membranes have been in contact with the blood, semen, or vaginal fluids of a defendant.
- When an exposed person has visible blood as a result of bites, i.e., a bite has drawn blood.
Maximizing Medical and Psychological Benefit to the Survivor
Exposure to HIV is an emergency. The sexual assault survivor should be evaluated in an emergency department as soon as possible for treatment and evaluation for PEP. The first dose of PEP medications should be administered as soon as possible—ideally within 2 hours of exposure and no later than 72 hours post-exposure. Studies have shown that the sooner PEP is initiated, the more likely it is to be effective.
A 28-day course of a 3-drug PEP regimen, as outlined in the NYSDOH AI guideline PEP to Prevent HIV Infection, should be prescribed if a sexual assault patient experienced a significant exposure to HIV. Clinicians are required by law to offer and make available a 7-day starter pack of HIV PEP to survivors of sexual assault who are ≥18 years old and offer and make available the full 28-day supply of HIV PEP to survivors of sexual assault who are <18 years old. Sexual assault patients should receive HIV testing at baseline (within 72 hours of the exposure) and at 4 weeks and 12 weeks post-exposure, even if PEP is declined, as detailed in the guideline (see Figure 4: Sexual Assault HIV Exposure: PEP and Exposure Management When Reported Within 72 Hours).
| New York State Law |
|
Court-Ordered HIV Testing of Defendants 7 to 30 Days from the Time of the Exposure
| PEP GUIDELINE RECOMMENDATION |
|
Rationale for the 7- to 30-day time frame: HIV can be detected as early as 7 days with an FDA-approved HIV-1/2 Ag/Ab combination test. After 30 days from the time of exposure, the survivor will have completed the 28-day PEP regimen; therefore, the testing recommendations change because the use of the HIV-1/2 Ag/Ab combination test in addition to the HIV RNA assay is not medically beneficial. See the section Court-Ordered HIV Testing of Defendants: 30 Days to 6 Months from the Time of the Exposure, below, for the psychological benefit that may be gained from defendant testing after 30 days.
Medical benefit for the survivor when testing the defendant between 7 and 30 days: The only clear medical benefit for the survivor of testing the defendant for HIV would be the discontinuation of PEP to avoid potential toxicity and adverse effects; for this benefit to be realized, the defendant’s test results would need to be available within the 28-day period for which the PEP regimen is prescribed.
The medical decision to discontinue PEP on the part of the survivor should be made only in full consultation with the survivor’s clinician. The survivor’s clinician should consult with a clinician experienced in managing PEP before discontinuing the regimen.
Psychological benefits of defendant testing for the sexual assault survivor: Defendant testing for HIV may have the following psychological benefits for the survivor:
- Providing information that may help the survivor understand the degree of risk for acquiring HIV.
- The comfort of knowing that exposure to HIV is unlikely in those instances when the defendant tests negative on both the HIV-1/2 Ag/Ab combination test and Ab differentiation assay.
- Allowing the survivor to participate more fully in the decision of whether to continue or discontinue the PEP regimen.
Expert consultation for New York State clinicians: Clinicians are advised to call the Clinical Education Initiative (CEI Line) to speak with an experienced HIV care provider.
- Call 1-866-637-2342, and press “2” for HIV.
- The CEI Line is available from 9 AM to 5 PM, Monday through Friday.
Because the results of the defendant’s test may be the only criterion used to decide to terminate the survivor’s PEP regimen, the committee concluded that it was necessary to exclude the possibility of the defendant being in the acute stage of HIV-1 infection. The acute stage is the stage in which the virus and viral RNA are present in the blood but the person has not developed enough specific antibodies to be detected by an antibody test. An HIV-1/2 Ag/Ab combination immunoassay may detect HIV-1 p24 antigen as early as 14 days and will also detect HIV-1 and HIV-2 antibodies produced once seroconversion has occurred. An HIV-1 RNA assay is capable of detecting HIV-1 as soon as 7 days after infection and would establish a diagnosis; therefore, it is important to use both an HIV-1/2 Ag/Ab combination immunoassay and a plasma HIV-1 RNA assay when the completion of the victim’s PEP regimen is contingent on the defendant test results. If the HIV antigen/antibody immunoassay is positive, the laboratory should complete the recommended HIV testing algorithm, which includes supplemental testing using an HIV-1/HIV-2 Ab differentiation test (see NYSDOH AI guideline HIV Testing). There is a robust body of evidence that individuals do not sexually transmit HIV if they are taking antiretroviral therapy (ART) and have an undetectable viral load (HIV RNA <200 copies/mL); see NYSDOH AI U=U Guidance for Implementation in Clinical Settings.
Negative test results from both the HIV-1/2 Ag/Ab combination immunoassay and the HIV-1 RNA assay would indicate that the defendant is not infected with HIV and would permit discontinuation of the survivor’s PEP regimen. Positive test results for either the HIV antibodies or HIV-1 RNA assay, or both, would indicate that the defendant has HIV and that the survivor’s PEP regimen should be completed. When making decisions regarding the management of the sexual assault survivor, the defendant should be considered to have HIV until proven otherwise. Table 1, below, outlines the different possibilities of test results, how each result would affect the survivor’s PEP regimen, and the necessary follow up.
| Abbreviations: Ab, antibody; Ag, antigen; PEP, post-exposure prophylaxis.
Note:
|
||
| Table 1: Follow-Up Based on Results of Defendant HIV Testing [a] Performed 7 to 30 Days Post-Sexual Assault | ||
| Defendant Test Results | Survivor PEP | Defendant Retesting and Follow-Up |
|
PEP may be discontinued after consultation with physician. |
|
|
PEP should be continued. |
|
|
PEP should be continued. |
|
|
PEP should be continued. |
|
| Inconclusive or invalid results from either the Ag/Ab or RNA assay. | PEP should be continued. | Repeat both tests as soon as possible in consultation with an HIV specialist. |
Court-Ordered HIV Testing of Defendants 30 Days to 6 Months from Time of Exposure
Recommended testing: When performing HIV testing of a defendant, clinicians should use the type of HIV test noted in Table 2, below, based on the amount of time that has passed since the assault:
- 30 days to 6 months post-assault: FDA-approved HIV-1/2 Ag/Ab combination immunoassay is recommended.
- 30 days to 42 days post-assault: Laboratory-based HIV-1/2 Ag/Ab combination immunoassay is recommended.
- 42 days to 6 months post-assault: Point-of-care rapid HIV test or a laboratory-based HIV-1/2 Ag/Ab combination immunoassay can be used.
Reactive results on any type of HIV screening assay should be confirmed in a laboratory using the recommended HIV testing algorithm (see the NYSDOH AI guideline HIV Testing).
Medical benefit for the survivor when testing the defendant between 30 days and 6 months: There is no medical benefit for the sexual assault survivor when testing the defendant for HIV during the 30-day to 6-month period. If the survivor chose to receive PEP, the 28-day PEP regimen will have been completed at this point. If the survivor tests negative at 12 weeks, then HIV transmission by exposure from the assault can be excluded.
Psychological benefits for the survivor when testing the defendant between 30 days and 6 months: Defendant testing for HIV that may be mandated by the court for up to 6 months after the assault can have the following psychological benefits for the survivor:
- Providing information that may help the survivor understand the degree of risk for acquiring HIV.
- The comfort of knowing that exposure to HIV is unlikely in those instances when the defendant tests HIV negative.
| Abbreviations: Ab, antibody; Ag, antigen.
Note:
|
|
| Table 2: Follow-Up Based on Results of Defendant HIV Testing [a] Performed 30 Days to 6 Months Post-Sexual Assault | |
| Defendant Test Results | Defendant Retesting and Follow-Up |
| Negative |
|
| Positive |
|
Responsibilities of the County or State Public Health Officer
If testing the defendant would provide medical benefit to the victim or a psychological benefit to the victim, then the testing is to be conducted by a state, county, or local public health officer designated by the order.
Responsibilities to the defendant:
- Provide pre-test information.
- Obtain appropriate HIV test(s), depending on the timing of testing in relation to when the exposure occurred.
- Provide post-test counseling.
Responsibilities to the sexual assault survivor:
- Notify the survivor of the defendant’s test results.
- Instruct the survivor to inform his/her healthcare provider of the results and discuss how to proceed with PEP.
Responsibility to the court: Notify the court in writing that the test(s) was performed and the results were shared with the sexual assault survivor.
Disclosure: Disclosure of confidential HIV-related information shall be made to the defendant upon his or her request.
- Disclosure to a person other than the defendant will be limited to the person making the application (i.e., the sexual assault survivor). The survivor may then disclose the defendant’s HIV test results to the survivor’s medical care provider, legal representative, and close family members or legal guardian. The survivor may also share the HIV-related information with his or her sex or needle-sharing partners if it is believed that these individuals were exposed to HIV.
- Survivors cannot disclose the defendant’s name during these discussions.
- Disclosure shall not be permitted to any other person or to the court.
Clinical Guidelines Program Approach to Shared Decision-Making
Download Printable PDF of Shared Decision-Making Statement
Date of current publication: August 8, 2023
Lead authors: Jessica Rodrigues, MS; Jessica M. Atrio, MD, MSc; and Johanna L. Gribble, MA
Writing group: Steven M. Fine, MD, PhD; Rona M. Vail, MD; Samuel T. Merrick, MD; Asa E. Radix, MD, MPH, PhD; Christopher J. Hoffmann, MD, MPH; Charles J. Gonzalez, MD
Committee: Medical Care Criteria Committee
Date of original publication: August 8, 2023
Rationale
Throughout its guidelines, the New York State Department of Health (NYSDOH) AIDS Institute (AI) Clinical Guidelines Program recommends “shared decision-making,” an individualized process central to patient-centered care. With shared decision-making, clinicians and patients engage in meaningful dialogue to arrive at an informed, collaborative decision about a patient’s health, care, and treatment planning. The approach to shared decision-making described here applies to recommendations included in all program guidelines. The included elements are drawn from a comprehensive review of multiple sources and similar attempts to define shared decision-making, including the Institute of Medicine’s original description [Institute of Medicine 2001]. For more information, a variety of informative resources and suggested readings are included at the end of the discussion.
Benefits
The benefits to patients that have been associated with a shared decision-making approach include:
- Decreased anxiety [Niburski, et al. 2020; Stalnikowicz and Brezis 2020]
- Increased trust in clinicians [Acree, et al. 2020; Groot, et al. 2020; Stalnikowicz and Brezis 2020]
- Improved engagement in preventive care [McNulty, et al. 2022; Scalia, et al. 2022; Bertakis and Azari 2011]
- Improved treatment adherence, clinical outcomes, and satisfaction with care [Crawford, et al. 2021; Bertakis and Azari 2011; Robinson, et al. 2008]
- Increased knowledge, confidence, empowerment, and self-efficacy [Chen, et al. 2021; Coronado-Vázquez, et al. 2020; Niburski, et al. 2020]
Approach
Collaborative care: Shared decision-making is an approach to healthcare delivery that respects a patient’s autonomy in responding to a clinician’s recommendations and facilitates dynamic, personalized, and collaborative care. Through this process, a clinician engages a patient in an open and respectful dialogue to elicit the patient’s knowledge, experience, healthcare goals, daily routine, lifestyle, support system, cultural and personal identity, and attitudes toward behavior, treatment, and risk. With this information and the clinician’s clinical expertise, the patient and clinician can collaborate to identify, evaluate, and choose from among available healthcare options [Coulter and Collins 2011]. This process emphasizes the importance of a patient’s values, preferences, needs, social context, and lived experience in evaluating the known benefits, risks, and limitations of a clinician’s recommendations for screening, prevention, treatment, and follow-up. As a result, shared decision-making also respects a patient’s autonomy, agency, and capacity in defining and managing their healthcare goals. Building a clinician-patient relationship rooted in shared decision-making can help clinicians engage in productive discussions with patients whose decisions may not align with optimal health outcomes. Fostering open and honest dialogue to understand a patient’s motivations while suspending judgment to reduce harm and explore alternatives is particularly vital when a patient chooses to engage in practices that may exacerbate or complicate health conditions [Halperin, et al. 2007].
Options: Implicit in the shared decision-making process is the recognition that the “right” healthcare decisions are those made by informed patients and clinicians working toward patient-centered and defined healthcare goals. When multiple options are available, shared decision-making encourages thoughtful discussion of the potential benefits and potential harms of all options, which may include doing nothing or waiting. This approach also acknowledges that efficacy may not be the most important factor in a patient’s preferences and choices [Sewell, et al. 2021].
Clinician awareness: The collaborative process of shared decision-making is enhanced by a clinician’s ability to demonstrate empathic interest in the patient, avoid stigmatizing language, employ cultural humility, recognize systemic barriers to equitable outcomes, and practice strategies of self-awareness and mitigation against implicit personal biases [Parish, et al. 2019].
Caveats: It is important for clinicians to recognize and be sensitive to the inherent power and influence they maintain throughout their interactions with patients. A clinician’s identity and community affiliations may influence their ability to navigate the shared decision-making process and develop a therapeutic alliance with the patient and may affect the treatment plan [KFF 2023; Greenwood, et al. 2020]. Furthermore, institutional policy and regional legislation, such as requirements for parental consent for gender-affirming care for transgender people or insurance coverage for sexual health care, may infringe upon a patient’s ability to access preventive- or treatment-related care [Sewell, et al. 2021].
Figure 1: Elements of Shared Decision-Making

Download figure: Elements of Shared Decision-Making
Health equity: Adapting a shared decision-making approach that supports diverse populations is necessary to achieve more equitable and inclusive health outcomes [Castaneda-Guarderas, et al. 2016]. For instance, clinicians may need to incorporate cultural- and community-specific considerations into discussions with women, gender-diverse individuals, and young people concerning their sexual behaviors, fertility intentions, and pregnancy or lactation status. Shared decision-making offers an opportunity to build trust among marginalized and disenfranchised communities by validating their symptoms, values, and lived experience. Furthermore, it can allow for improved consistency in patient screening and assessment of prevention options and treatment plans, which can reduce the influence of social constructs and implicit bias [Castaneda-Guarderas, et al. 2016].
Clinician bias has been associated with health disparities and can have profoundly negative effects [FitzGerald and Hurst 2017; Hall, et al. 2015]. It is often challenging for clinicians to recognize and set aside personal biases and to address biases with peers and colleagues. Consciously or unconsciously, negative or stigmatizing assumptions are often made about patient characteristics, such as race, ethnicity, gender, sexual orientation, mental health, and substance use [Avery, et al. 2019; van Boekel, et al. 2013; Livingston, et al. 2012]. With its emphasis on eliciting patient information, a shared decision-making approach encourages clinicians to inquire about patients’ lived experiences rather than making assumptions and to recognize the influence of that experience in healthcare decision-making.
Stigma: Stigma may prevent individuals from seeking or receiving treatment and harm reduction services [Tsai, et al. 2019]. Among people with HIV, stigma and medical mistrust remain significant barriers to healthcare utilization, HIV diagnosis, and medication adherence and can affect disease outcomes [Turan, et al. 2017; Chambers, et al. 2015], and stigma among clinicians against people who use substances has been well-documented [Stone, et al. 2021; Tsai, et al. 2019; van Boekel, et al. 2013]. Sexual and reproductive health, including strategies to prevent HIV transmission, acquisition, and progression, may be subject to stigma, bias, social influence, and violence.
| SHARED DECISION-MAKING IN HIV CARE |
|
Resources and Suggested Reading
In addition to the references cited below, the following resources and suggested reading may be useful to clinicians.
| RESOURCES |
References
Acree ME, McNulty M, Blocker O, et al. Shared decision-making around anal cancer screening among black bisexual and gay men in the USA. Cult Health Sex 2020;22(2):201-16. [PMID: 30931831]
Avery JD, Taylor KE, Kast KA, et al. Attitudes toward individuals with mental illness and substance use disorders among resident physicians. Prim Care Companion CNS Disord 2019;21(1):18m02382. [PMID: 30620451]
Bertakis KD, Azari R. Patient-centered care is associated with decreased health care utilization. J Am Board Fam Med 2011;24(3):229-39. [PMID: 21551394]
Castaneda-Guarderas A, Glassberg J, Grudzen CR, et al. Shared decision making with vulnerable populations in the emergency department. Acad Emerg Med 2016;23(12):1410-16. [PMID: 27860022]
Chambers LA, Rueda S, Baker DN, et al. Stigma, HIV and health: a qualitative synthesis. BMC Public Health 2015;15:848. [PMID: 26334626]
Chen CH, Kang YN, Chiu PY, et al. Effectiveness of shared decision-making intervention in patients with lumbar degenerative diseases: a randomized controlled trial. Patient Educ Couns 2021;104(10):2498-2504. [PMID: 33741234]
Coronado-Vázquez V, Canet-Fajas C, Delgado-Marroquín MT, et al. Interventions to facilitate shared decision-making using decision aids with patients in primary health care: a systematic review. Medicine (Baltimore) 2020;99(32):e21389. [PMID: 32769870]
Coulter A, Collins A. Making shared decision-making a reality: no decision about me, without me. 2011. https://www.kingsfund.org.uk/sites/default/files/Making-shared-decision-making-a-reality-paper-Angela-Coulter-Alf-Collins-July-2011_0.pdf
Crawford J, Petrie K, Harvey SB. Shared decision-making and the implementation of treatment recommendations for depression. Patient Educ Couns 2021;104(8):2119-21. [PMID: 33563500]
FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics 2017;18(1):19. [PMID: 28249596]
Greenwood BN, Hardeman RR, Huang L, et al. Physician-patient racial concordance and disparities in birthing mortality for newborns. Proc Natl Acad Sci U S A 2020;117(35):21194-21200. [PMID: 32817561]
Groot G, Waldron T, Barreno L, et al. Trust and world view in shared decision making with indigenous patients: a realist synthesis. J Eval Clin Pract 2020;26(2):503-14. [PMID: 31750600]
Hall WJ, Chapman MV, Lee KM, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health 2015;105(12):e60-76. [PMID: 26469668]
Halperin B, Melnychuk R, Downie J, et al. When is it permissible to dismiss a family who refuses vaccines? Legal, ethical and public health perspectives. Paediatr Child Health 2007;12(10):843-45. [PMID: 19043497]
Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. 2001. https://www.ncbi.nlm.nih.gov/books/NBK222274/
KFF. Key data on health and health care by race and ethnicity. 2023 Mar 15. https://www.kff.org/racial-equity-and-health-policy/report/key-data-on-health-and-health-care-by-race-and-ethnicity/ [accessed 2023 May 19]
Livingston JD, Milne T, Fang ML, et al. The effectiveness of interventions for reducing stigma related to substance use disorders: a systematic review. Addiction 2012;107(1):39-50. [PMID: 21815959]
McNulty MC, Acree ME, Kerman J, et al. Shared decision making for HIV pre-exposure prophylaxis (PrEP) with black transgender women. Cult Health Sex 2022;24(8):1033-46. [PMID: 33983866]
Niburski K, Guadagno E, Abbasgholizadeh-Rahimi S, et al. Shared decision making in surgery: a meta-analysis of existing literature. Patient 2020;13(6):667-81. [PMID: 32880820]
Parish SJ, Hahn SR, Goldstein SW, et al. The International Society for the Study of Women’s Sexual Health process of care for the identification of sexual concerns and problems in women. Mayo Clin Proc 2019;94(5):842-56. [PMID: 30954288]
Robinson JH, Callister LC, Berry JA, et al. Patient-centered care and adherence: definitions and applications to improve outcomes. J Am Acad Nurse Pract 2008;20(12):600-607. [PMID: 19120591]
Scalia P, Durand MA, Elwyn G. Shared decision-making interventions: an overview and a meta-analysis of their impact on vaccine uptake. J Intern Med 2022;291(4):408-25. [PMID: 34700363]
Sewell WC, Solleveld P, Seidman D, et al. Patient-led decision-making for HIV preexposure prophylaxis. Curr HIV/AIDS Rep 2021;18(1):48-56. [PMID: 33417201]
Stalnikowicz R, Brezis M. Meaningful shared decision-making: complex process demanding cognitive and emotional skills. J Eval Clin Pract 2020;26(2):431-38. [PMID: 31989727]
Stone EM, Kennedy-Hendricks A, Barry CL, et al. The role of stigma in U.S. primary care physicians’ treatment of opioid use disorder. Drug Alcohol Depend 2021;221:108627. [PMID: 33621805]
Tsai AC, Kiang MV, Barnett ML, et al. Stigma as a fundamental hindrance to the United States opioid overdose crisis response. PLoS Med 2019;16(11):e1002969. [PMID: 31770387]
Turan B, Budhwani H, Fazeli PL, et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav 2017;21(1):283-91. [PMID: 27272742]
van Boekel LC, Brouwers EP, van Weeghel J, et al. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend 2013;131(1-2):23-35. [PMID: 23490450]
NYSDOH HIV Care Provider Definitions
Throughout HIV-related guidelines and other materials, when reference is made to “experienced HIV care provider” or “expert HIV care provider,” those terms are referring to the following 2017 NYSDOH AI definitions:
- Experienced HIV care provider: Practitioners who have been accorded HIV Experienced Provider status by the American Academy of HIV Medicine or have met the HIV Medicine Association’s definition of an experienced provider are eligible for designation as an HIV Experienced Provider in New York State. Nurse practitioners and licensed midwives who provide clinical care to individuals with HIV in collaboration with a physician may be considered HIV Experienced Providers as long as all other practice agreements are met (8 NYCRR 79-5:1; 10 NYCRR 85.36; 8 NYCRR 139-6900). Physician assistants who provide clinical care to individuals with HIV under the supervision of an HIV Specialist physician may also be considered HIV Experienced Providers (10 NYCRR 94.2)
- Expert HIV care provider: A provider with extensive experience in the management of complex patients with HIV.
Use of Dolutegravir in Individuals of Childbearing Capacity
Lead author: Geoffrey A. Weinberg, MD, with the Medical Care Criteria Committee; May 2021
Potentially increased NTDs and DTG: NTDs are birth defects, including meningomyelocele and spina bifida, thought to occur early after conception during development of the embryonic neural tube. The neural tube closes by approximately 8 weeks gestational age, which is 8 weeks after the last menstrual period or approximately 6 weeks post-conception. Ingestion of folic acid or folate by a pregnant individual significantly lowers the rate of NTDs; all individuals in the United States who are pregnant or trying to conceive and engaged in prenatal care are routinely administered 400 µg of folic acid daily. The background rate of NTDs in the general population in the United States and other countries that routinely fortify food with folate or folic acid is low: approximately 0.07% of all births (7/10,000 births) [Reefhuis, et al. 2020].
In 2018, an unplanned interim analysis of a large observational clinical trial conducted in Botswana, a country where food is not routinely fortified with folate or folic acid, was performed. The researchers found NTDs in 0.94% of 426 infants exposed at conception to maternal DTG-based antiretroviral therapy (ART) compared with 0.12% of 11,300 infants exposed to non–DTG-based ART. Importantly, however, as more data were collected, the rates of infant NTDs markedly declined [Antiretroviral Pregnancy Registry Steering Committee 2022; DHHS 2022; Zash 2020; Zash, et al. 2019; Zash, et al. 2018]. The latest available data, through April 2020, now show that the rate of infant NTDs with maternal DTG-based ART use at conception is not any greater than it is in infants exposed to non–DTG-based ART at conception: 0.19% [Antiretroviral Pregnancy Registry Steering Committee 2022; DHHS 2022; Zash 2020]. No increases have been found in the registry data or through pharmacovigilance database studies from Europe and the United States [van De Ven, et al. 2020; Vannappagari and Thorne 2019]. Nor have any differences been found in the rates of NTDs among infants in a randomized controlled open-label phase 3 trial of DTG-based versus EFV-based ART in pregnant individuals, though the median gestational age at enrollment in this trial was 22 weeks, and all enrollees were at 14 weeks or more gestational age at enrollment [Lockman, et al. 2021].
Benefits of DTG: There are many known benefits of DTG as a component of ART for all adults, pregnant or not, and many children. DTG is potent, rapidly reduces viral load, has a high barrier to HIV genetic resistance, and is generally well-tolerated. Moreover, folate deficiency is uncommon in countries such as the United States. Thus, both the U.S. Department of Health and Human Services and the World Health Organization consider DTG a preferred ARV drug for individuals with HIV in all trimesters of pregnancy, and those with HIV who are trying to conceive. If an alternative ART regimen that does not include DTG is the best choice, alternatives to DTG during pregnancy include raltegravir, ritonavir-boosted atazanavir, or ritonavir-boosted darunavir (see the NYSDOH AI guideline Selecting an Initial ART Regimen > Specific Factors to Consider and Discuss With Patients). No data currently exist to support the use of bictegravir during pregnancy or the period surrounding conception. Further, cobicistat-boosted regimens containing elvitegravir, darunavir, or atazanavir are not recommended due to reduced levels of the integrase inhibitors given with cobicistat during pregnancy.
References
Antiretroviral Pregnancy Registry Steering Committee. Antiretroviral Pregnancy Registry Interim Report for 1 January 1989 – 31 July 2022. 2022 Dec 19. http://apregistry.com/forms/exec-summary.pdf [accessed 2021 Apr 19]
DHHS. Recommendations for the Use of Antiretroviral Drugs During Pregnancy and Interventions to Reduce Perinatal HIV Transmission in the United States. 2022 Mar 17. https://clinicalinfo.hiv.gov/en/guidelines/perinatal/whats-new-guidelines [accessed 2021 Apr 19]
Lockman S, Brummel SS, Ziemba L, et al. Efficacy and safety of dolutegravir with emtricitabine and tenofovir alafenamide fumarate or tenofovir disoproxil fumarate, and efavirenz, emtricitabine, and tenofovir disoproxil fumarate HIV antiretroviral therapy regimens started in pregnancy (IMPAACT 2010/VESTED): a multicentre, open-label, randomised, controlled, phase 3 trial. Lancet 2021;397(10281):1276-1292. [PMID: 33812487]
Reefhuis J, FitzHarris LF, Gray KM, et al. Neural tube defects in pregnancies among women with diagnosed HIV infection – 15 jurisdictions, 2013-2017. MMWR Morb Mortal Wkly Rep 2020;69(1):1-5. [PMID: 31917782]
van De Ven NS, Pozniak AL, Levi JA, et al. Analysis of pharmacovigilance databases for dolutegravir safety in pregnancy. Clin Infect Dis 2020;70(12):2599-2606. [PMID: 31595301]
Vannappagari V, Thorne C. Pregnancy and neonatal outcomes following prenatal exposure to dolutegravir. J Acquir Immune Defic Syndr 2019;81(4):371-378. [PMID: 30939532]
Zash R. Update on neural tube defects with antiretroviral exposure in the Tsepamo study, Botswana. IAC; 2020 Jul 6-10; Virtual. https://www.natap.org/2020/IAC/IAC_112.htm
Zash R, Holmes L, Diseko M, et al. Neural-tube defects and antiretroviral treatment regimens in Botswana. N Engl J Med 2019;381(9):827-840. [PMID: 31329379]
Zash R, Makhema J, Shapiro RL. Neural-tube defects with dolutegravir treatment from the time of conception. N Engl J Med 2018;379(10):979-981. [PMID: 30037297]
GOALS Framework for Sexual History Taking in Primary Care
Download Printable PDF of GOALS Framework
Date of current publication: September 26, 2023
Lead author: Sarit A. Golub, PhD, MPH, Hunter College and Graduate Center, City University of New York, in collaboration with the New York City Department of Health and Mental Hygiene, Bureau of HIV
Date of original publication: July 30, 2019
Background: Sexual history taking can be an onerous and awkward task that does not always provide accurate or useful information for patient care. Standard risk assessment questions (e.g., How many partners have you had sex within the last 6 months?; How many times did you have receptive anal sex with a man when he did not use a condom?) may be alienating to patients, discourage honest disclosure, and communicate that the number of partners or acts is the only component of sexual risk and health.
In contrast, the GOALS framework is designed to streamline sexual history conversations and elicit information most useful for identifying an appropriate clinical course of action. The “goal” of the GOALS framework is to reimagine the sexual history to make it easier and more productive for providers and patients.
The GOALS framework was developed in response to 4 key findings from the sexual health research literature:
- Universal HIV/STI screening and biomedical prevention education is more beneficial and cost-effective than risk-based screening [Eckman, et al. 2021; Keenan, et al. 2020; Lancki, et al. 2018; Hull, et al. 2017; Hoots, et al. 2016; Owusu-Edusei, et al. 2016].
- Emphasizing benefits—rather than risks—is more successful in motivating patients toward prevention and care behavior [Reynolds-Tylus 2019; Epton, et al. 2015; Sheeran, et al. 2014; Weinstein and Klein 1995].
- Positive interactions with healthcare providers promote engagement in prevention and care [Howe, et al. 2019; Flickinger, et al. 2013; Alexander, et al. 2012; Bakken, et al. 2000].
- Patients want their healthcare providers to talk with them about sexual health [Agochukwu-Mmonu, et al. 2021; Zhang, et al. 2020; Ryan, et al. 2018; Fairchild, et al. 2016].
Rather than seeing sexual history taking as a means to an end, the GOALS framework considers the sexual history taking process as an intervention that can:
- Increase rates of routine HIV/STI screening;
- Increase rates of universal biomedical prevention and contraceptive education;
- Increase patients’ motivation for and commitment to sexual health behavior; and
- Enhance the patient-care provider relationship, making it a lever for sexual health specifically and overall wellness.
The GOALS framework includes 5 steps:
- Give a preamble that emphasizes sexual health. The healthcare provider briefly introduces the sexual history in a way that de-emphasizes risk, normalizes sexuality as part of routine healthcare, and opens the door for the patient’s questions.
- Offer opt-out HIV/STI testing and information. The healthcare provider tells the patient that they test everyone for HIV and STIs, normalizing both testing and HIV and STI concerns.
- Ask an open-ended question. The healthcare provider starts the sexual history with an open-ended question that helps them identify the aspects of sexual health that are most important to the patient, while allowing them to hear (and then mirror) the language that the patient uses to describe their own body, partner(s), and sexual behaviors.
- Listen for relevant information and fill in the blanks. The healthcare provider asks more pointed questions to elicit information that might be needed for clinical decision-making (e.g., 3-site versus genital-only testing), but these questions are restricted to specific, necessary information. For instance, if a patient has already disclosed that he is a gay man with more than 1 partner, there is no need to ask about the total number of partners or their HIV status to recommend STI/HIV testing and pre-exposure prophylaxis (PrEP) education.
- Suggest a course of action. Consistent with opt-out testing, the healthcare provider offers all patients HIV testing, 3-site STI testing, PrEP education, and contraceptive counseling, unless any of this testing is specifically contraindicated by the sexual history. Rather than focusing on any risk behaviors the patient may be engaging in, this step focuses specifically on the benefits of engaging in prevention behaviors, such as exerting greater control over one’s sex life and sexual health and decreasing anxiety about potential transmission.
Resources for implementation:
- Script, rationale, and goals: Box 1, below, provides a suggested script for each step in the GOALS framework, along with the specific rationale for that step and the goal it is designed to accomplish.
- GOALS Three-Part Video Series (NIH-funded BLUPrInt Project)
- Reimagining the Sexual History, GOALS Approach Evidence and Elements, and Taking Risk Out of the Pitch (AETC): A self-paced, interactive, online training
- The 5Ps model for sexual history-taking (CDC): Note that the GOALS framework is not necessarily designed to replace the 5Ps model (partners, practices, protection from STI, history of STI, prevention of pregnancy); instead, it provides a framework for identifying information related to the 5Ps that improves patient-care provider communication, reduces the likelihood of bias or missed opportunities, and enhances patients’ motivation for prevention and sexual health behavior.
| Box 1: GOALS Framework for the Sexual History |
||
| Component | Suggested Script | Rationale and Goal Accomplished |
| Give a preamble that emphasizes sexual health. | I’d like to talk with you for a couple of minutes about your sexuality and sexual health. I talk to all of my patients about sexual health, because it’s such an important part of overall health. Some of my patients have questions or concerns about their sexual health, so I want to make sure I understand what your questions or concerns might be and provide whatever information or other help you might need. |
|
| Offer opt-out HIV/STI testing and information. | First, I like to test all my patients for HIV and other sexually transmitted infections. Do you have any concerns about that? |
|
| Ask an open-ended question. | Pick one (or use an open-ended question that you prefer):
|
|
| Listen for relevant information and probe to fill in the blanks. |
|
|
| Suggest a course of action. |
|
|
Download Box 1: GOALS Framework for the Sexual History Printable PDF
References
Agochukwu-Mmonu N, Malani PN, Wittmann D, et al. Interest in sex and conversations about sexual health with health care providers among older U.S. adults. Clin Gerontol 2021;44(3):299-306. [PMID: 33616005]
Alexander JA, Hearld LR, Mittler JN, et al. Patient-physician role relationships and patient activation among individuals with chronic illness. Health Serv Res 2012;47(3 Pt 1):1201-23. [PMID: 22098418]
Bakken S, Holzemer WL, Brown MA, et al. Relationships between perception of engagement with health care provider and demographic characteristics, health status, and adherence to therapeutic regimen in persons with HIV/AIDS. AIDS Patient Care STDS 2000;14(4):189-97. [PMID: 10806637]
Eckman MH, Reed JL, Trent M, et al. Cost-effectiveness of sexually transmitted infection screening for adolescents and young adults in the pediatric emergency department. JAMA Pediatr 2021;175(1):81-89. [PMID: 33136149]
Epton T, Harris PR, Kane R, et al. The impact of self-affirmation on health-behavior change: a meta-analysis. Health Psychol 2015;34(3):187-96. [PMID: 25133846]
Fairchild PS, Haefner JK, Berger MB. Talk about sex: sexual history-taking preferences among urogynecology patients and general gynecology controls. Female Pelvic Med Reconstr Surg 2016;22(5):297-302. [PMID: 27171322]
Flickinger TE, Saha S, Moore RD, et al. Higher quality communication and relationships are associated with improved patient engagement in HIV care. J Acquir Immune Defic Syndr 2013;63(3):362-66. [PMID: 23591637]
Hoots BE, Finlayson T, Nerlander L, et al. Willingness to take, use of, and indications for pre-exposure prophylaxis among men who have sex with men-20 US cities, 2014. Clin Infect Dis 2016;63(5):672-77. [PMID: 27282710]
Howe LC, Leibowitz KA, Crum AJ. When your doctor “gets it” and “gets you”: the critical role of competence and warmth in the patient-provider interaction. Front Psychiatry 2019;10:475. [PMID: 31333518]
Hull S, Kelley S, Clarke JL. Sexually transmitted infections: compelling case for an improved screening strategy. Popul Health Manag 2017;20(S1):s1-11. [PMID: 28920768]
Keenan M, Thomas P, Cotler K. Increasing sexually transmitted infection detection through screening at extragenital sites. J Nurs Pract 2020;16(2):e27-30. https://doi.org/10.1016/j.nurpra.2019.07.023
Lancki N, Almirol E, Alon L, et al. Preexposure prophylaxis guidelines have low sensitivity for identifying seroconverters in a sample of young Black MSM in Chicago. AIDS 2018;32(3):383-92. [PMID: 29194116]
Owusu-Edusei K, Jr., Hoover KW, Gift TL. Cost-effectiveness of opt-out chlamydia testing for high-risk young women in the U.S. Am J Prev Med 2016;51(2):216-24. [PMID: 26952078]
Reynolds-Tylus T. Psychological reactance and persuasive health communication: a review of the literature. Frontiers in Communication 2019;4. https://www.frontiersin.org/articles/10.3389/fcomm.2019.00056
Ryan KL, Arbuckle-Bernstein V, Smith G, et al. Let’s talk about sex: a survey of patients’ preferences when addressing sexual health concerns in a family medicine residency program office. PRiMER 2018;2:23. [PMID: 32818195]
Sheeran P, Harris PR, Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychol Bull 2014;140(2):511-43. [PMID: 23731175]
Weinstein ND, Klein WM. Resistance of personal risk perceptions to debiasing interventions. Health Psychol 1995;14(2):132-40. [PMID: 7789348]
Zhang X, Sherman L, Foster M. Patients’ and providers’ perspectives on sexual health discussion in the United States: a scoping review. Patient Educ Couns 2020;103(11):2205-13. [PMID: 32601041]
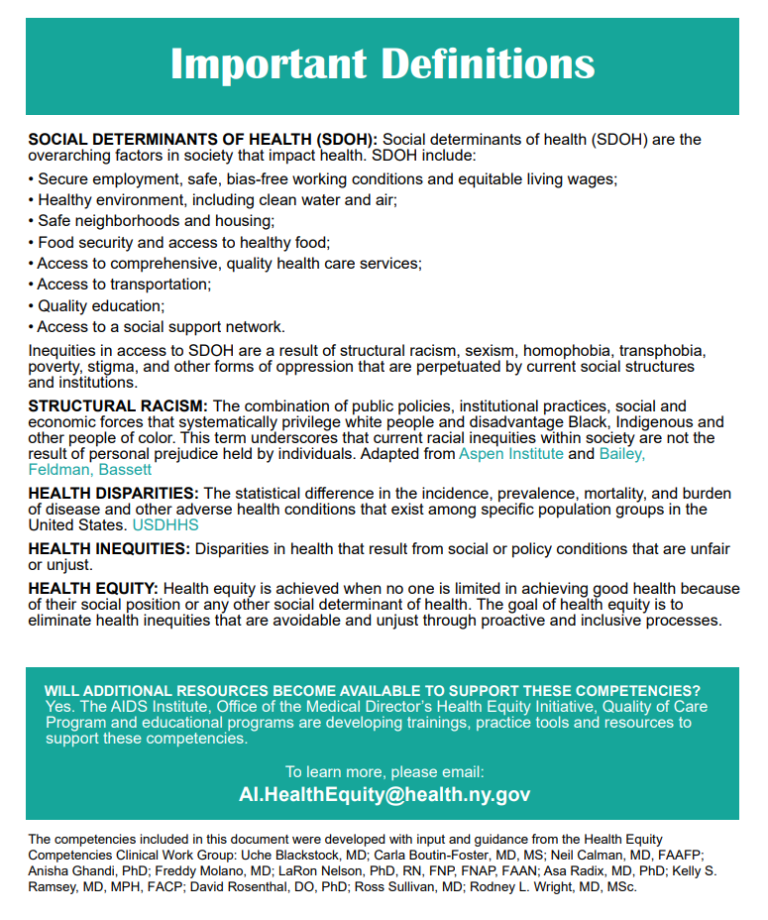
NYSDOH Health Equity Competencies for Health Care Providers
August 2021
Download Printable PDF of Health Equity Competencies
Health Equity Competencies Page 1
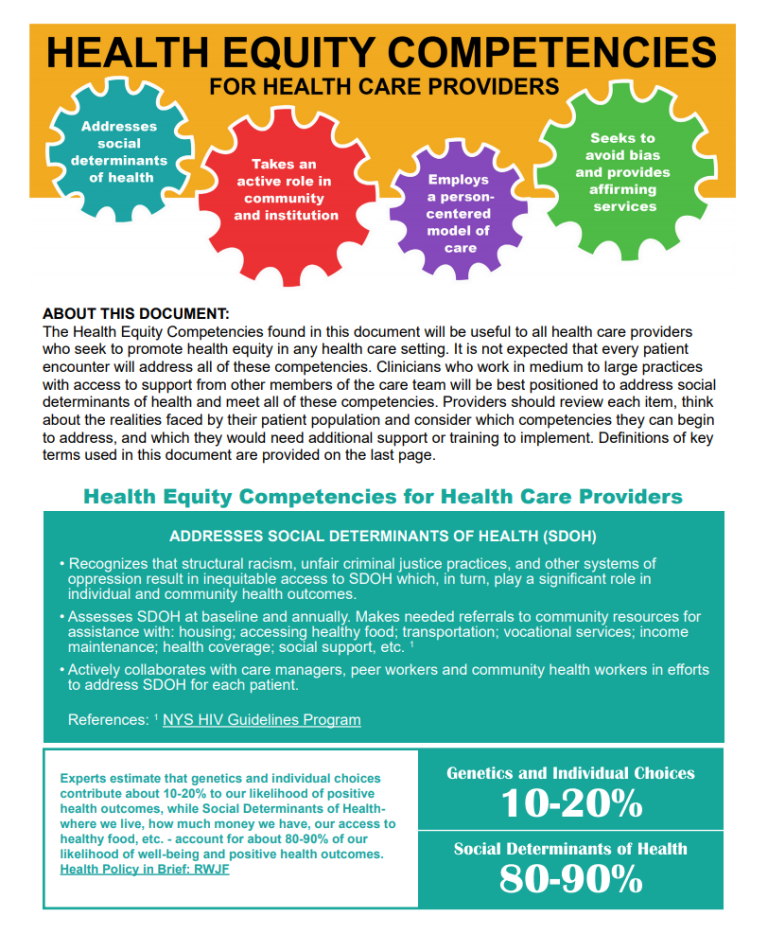
Health Equity Competencies Page 2
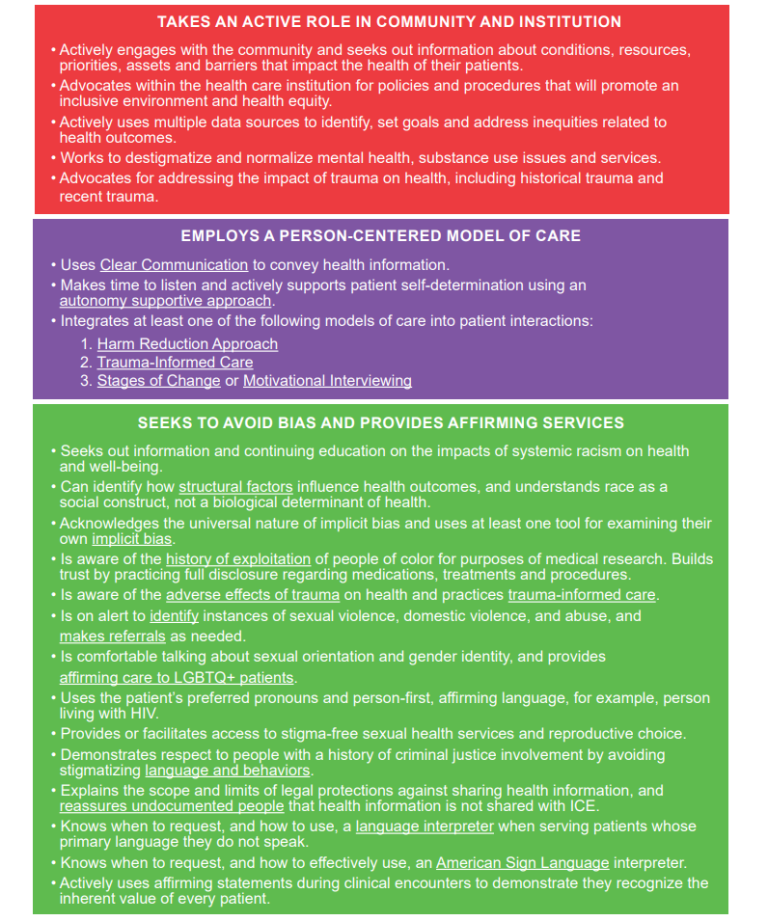
Health Equity Competencies Page 3
Selected Links: Resources for Clinicians
June 2022
New York State Department of Health:
- AIDS Institute Provider Directory (HIV, HCV, PEP, PrEP, Emergency PEP Located at a Pharmacy, Buprenorphine, STI Services, Opioid Overdose Prevention Program)
- AIDS Institute Training Centers
- Beyond Status
- Clinical Education Initiative (CEI): HIV Primary Care and Prevention, Sexual Health, HCV Treatment, and Drug User Health
- CEI: PrEP/PEP Resources
- CEI: PEP, PrEP, and HCV Clinical Cards (to attach to name badges; available for NYS care providers)
- Communicable Disease Reporting
- Court-Ordered HIV Testing of Defendants
- Emergency Contraception: What You Need to Know
- Ending the AIDS Epidemic in New York State
- Expedited Partner Therapy
- HIV/AIDS Testing, Reporting and Confidentiality of HIV-Related Information
- HIV/AIDS Laws & Regulations
- HIV Testing, Reporting and Confidentiality in New York State 2017-18 Update: Fact Sheet and Frequently Asked Questions
- Informed Consent for HIV Testing and Access to HIV Care for Adolescents
- Medicaid Coverage for HIV PrEP-Related Services
- Occupational Exposure and HIV Testing FAQ
- Partner Services: What Health Care Providers Need to Know
- Payment Options for Adults and Adolescents for Post Exposure Prophylaxis Following Sexual Assault
- Payment Options for Post‐Exposure Prophylaxis Following Non‐Occupational Exposures Including Sexual Assault
- PrEP and PEP Information & Resources
- PrEP Provider Directory
- PrEP for Sex
- Provider Reporting & Partner Services
- Rape Crisis Programs by County
- Rapid Testing for HIV
- Requirements to Report Instances of Suspected Child Abuse or Maltreatment
- Rules, Regulations & Laws
- Sexual Violence Prevention Program
- Sexual Assault Forensic Examiner (SAFE) Program
- Sexually Transmitted Infections
- STI Self-Collection Outside of a Clinic Setting in New York State (NYS) Question & Answer
- Truvada and Descovy Medicaid Fee-for-Service
- Uninsured Care Programs
- Wadsworth Center (HIV-1/2 adult and pediatric testing)
- What Health Care Providers Need to Know About Partner Services
- What Support Services Providers Should Know About HIV Clinical Guidelines: PrEP to Prevent HIV and Promote Sexual Health
New York State:
- Child Abuse Medical Provider Program > Education for Child Abuse Medical Providers
- eHealth Collaborative
- Expanded HIV Testing website
- Office for the Prevention of Domestic Violence
- Office of Victim Services
- Safety and Health
- Workers’ Compensation Board: Information for Health Care Providers
New York City:
- Alliance Against Sexual Assault
- Contact Notification Assistance Program (CNAP)
- Expedited Partner Therapy
- Reporting Diseases and Conditions
- Sexual Health Clinics
- Where to Get PrEP and PEP in New York City
AIDS Education & Training Center: National HIV Curriculum
Centers for Disease Control and Prevention:
- Post-Exposure Prophylaxis
- Preventing Needlestick Injuries in Health Care Settings
- PrEP Resources for Care Providers
Clinical Info HIV.gov: Drug Database
Gay & Lesbian Medical Association: Guidelines for Care of Lesbian, Gay, Bisexual, and Transgender Patients
HIV-ASSIST: Free Clinical Decision-Making Support for ARV Selection
Infectious Diseases Society of America: Diagnosis of Infectious Diseases
National Coalition for Sexual Health:
- A New Approach to Sexual History Taking: Talking About Pleasure, Problems, and Pride During a Sexual History (videos)
- Sexual Health and Your Patients: A Provider’s Guide
NASTAD: PrEP Coverage Brief: PrEP Services Covered With No Cost Sharing
PleasePrEPme.org: Provider Resources
University of California San Francisco (UCSF):
- Clinician Consultation Center: Post-Exposure Prophylaxis
- Pre-Exposure Prophylaxis Phone Consultation
University of Liverpool: HIV Drug Interactions
U.S. Department of Labor Occupational Safety and Health Administration (OSHA):
Selected Links: Resources for Consumers
June 2022
AIDS Institute Clinical Guidelines Program:
- PrEP Payment Options
- I Might Have Been Exposed . . . What Should I Do?
- Podría Haber Estado Eexpuesto al VIH… ¿Qué Debo Hacer?
New York State Department of Health:
- AIDS Institute Provider Directory (HIV, HCV, PEP, PrEP, Emergency PEP Located at a Pharmacy, Buprenorphine, STI Services, Opioid Overdose Prevention Program)
- Beyond Status
- Emergency Contraception: What You Need to Know
- Expedited Partner Therapy
- Health Insurance Portability and Accountability Act (HIPAA)
- HIV Testing
- HIV/AIDS Testing, Reporting and Confidentiality of HIV-Related Information
- HIV/AIDS Basics & Other Resources
- HIV/AIDS and STD Testing
- How Informed Consent for HIV Testing, HIV Partner Notification by Health Department Staff and Access to HIV Primary Care are Handled when a Minor is Involved
- NYS Medicaid Coverage for HIV Pre-Exposure Prophylaxis (PrEP) Related Services
- Payment Options for Adults and Adolescents for Post Exposure Prophylaxis Following Sexual Assault
- Payment Options for Post‐Exposure Prophylaxis Following Non‐Occupational Exposures Including Sexual Assault
- Post-Exposure Prophylaxis (PEP)
- PrEP and PEP Information & Resources
- Preventing HIV by Taking One Pill Once a Day: Pre-exposure Prophylaxis (PrEP) FAQs
- Provider Reporting & Partner Services
- Rape Crisis Programs by County
- Sexual Violence Prevention Program
- Sexually Transmitted Infections
- STD Clinics in New York State
- Truvada and Descovy Medicaid Fee-for-Service
- What is PEP? Fact Sheet
- YGetIt? Project
New York State:
- Coalition Against Sexual Assault
- Office for the Prevention of Domestic Violence
- Office of Victim Services
- Safety and Health
- Sexual Assault Victim Bill of Rights
- Workers’ Compensation Board: Information for Health Care Providers
New York City:
American College of Obstetricians and Gynecologists (ACOG): Preventing HIV With Medication FAQ
Centers for Disease Control and Prevention:
- HIV Risk Reduction Tool
- Post-Exposure Prophylaxis
- Preventing Needlestick Injuries in Health Care Settings
- PrEP (Pre-Exposure Prophylaxis)
- PrEP 101
HIV.gov:
Migrant Clinicians Network: Sexual Assault
NAM Aidsmap: Post-Exposure Prophylaxis (PEP)
New York-Presbyterian/Columbia University Medical Center: Domestic and Other Violence Emergencies (DOVE)
PrEP Locator: Find Your Provider
PrEPWatch
University of California San Francisco (UCSF): PrEP for U.S. Trans Women
U.S. Department of Labor Occupational Safety and Health Administration (OSHA):
All FDA-Approved HIV Medications, With Brand Names and Abbreviations
Reviewed April 2024
Listed below are all FDA-approved HIV medications as of March 23, 2023, per HIVinfo.NIH.gov, with links to the Clinical Info HIV.gov drug database. The list is organized by drug class, with individual drugs listed in alphabetical order. Combination drugs are also listed in alphabetical order.
Nucleoside Reverse Transcriptase Inhibitors (NRTIs): characteristics
- Abacavir (ABC; Ziagen): FDA label | Patient info
- Emtricitabine (FTC; Emtriva): FDA label | Patient info
- Lamivudine (3TC; Epivir): FDA label | Patient info
- Tenofovir Disoproxil Fumarate (TDF; Viread): FDA label | Patient info
- Zidovudine (AZT, ZDV; Retrovir): FDA label | Patient info
Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs): characteristics
- Doravirine (DOR; Pifeltro): FDA label | Patient info
- Efavirenz (EFV; Sustiva): FDA label | Patient info
- Etravirine (ETR; Intelence): FDA label | Patient info
- Nevirapine (NVP; Viramune, Viramune XR [extended release]): FDA label | Patient info
- Rilpivirine (RPV; Edurant): FDA label | Patient info
Protease Inhibitors (PIs): characteristics
- Atazanavir (ATV; Reyataz): FDA label | Patient info
- Darunavir (DRV; Prezista): FDA label | Patient info
- Fosamprenavir (FPV; Lexiva): FDA label | Patient info
- Ritonavir (RTV; Norvir): FDA label | Patient info
- Tipranavir (TPV; Aptivus): FDA label | Patient info
Fusion Inhibitor: characteristics
- Enfuvirtide (T-20; Fuzeon): FDA label | Patient info
CCR5 Antagonist: characteristics
- Maraviroc (MVC; Selzentry): FDA label | Patient info
Integrase Strand Transfer Inhibitors (INSTIs): characteristics
- Cabotegravir (CAB; Vocabria): FDA label | Patient info
- Dolutegravir (DTG; Tivicay): FDA label | Patient info
- Raltegravir (RAL; Isentress, Isentress HD): FDA label | Patient info
Attachment Inhibitor: characteristics
- Fostemsavir (FTR; Rukobia): FDA label | Patient info
Post-Attachment Inhibitor: characteristics
- Ibalizumab-uiyk (IBA; Trogarzo): FDA label | Patient info
Capsid Inhibitor: characteristics
- Lenacapavir (LEN; Sunlenca): FDA label | Patient info
Pharmacokinetic Enhancer: characteristics
- Cobicistat (COBI; Tybost): FDA label | Patient info
Combination HIV Medications:
- Abacavir/Lamivudine (ABC/3TC; Epzicom): FDA label | Patient info
- Abacavir/Dolutegravir/Lamivudine (ABC/DTG/3TC; Triumeq, Triumeq PD): FDA label | Patient info
- Abacavir/Lamivudine/Zidovudine (ABC/3TC/ZDV; Trizivir): FDA label | Patient info
- Atazanavir/Cobicistat (ATV/COBI; Evotaz): FDA label | Patient info
- Bictegravir/Emtricitabine/Tenofovir Alafenamide Fumarate (BIC/FTC/TAF; Biktarvy): FDA label | Patient info
- Cabotegravir/Rilpivirine (CAB/RPV; Cabenuva): FDA label | Patient info
- Darunavir/Cobicistat (DRV/COBI; Prezcobix): FDA label | Patient info
- Darunavir/Cobicistat/Emtricitabine/Tenofovir Alefenamide (DRV/COBI/FTC/TAF; Symtuza): FDA label | Patient info
- Dolutegravir/Lamivudine (DTG/3TC; Dovato): FDA label | Patient info
- Dolutegravir/Rilpivirine (DTG/RPV; Juluca): FDA label | Patient info
- Doravirine/Lamivudine/Tenofovir Disoproxil Fumarate (DOR/3TC/TDF; Delstrigo): FDA label | Patient info
- Efavirenz/Emtricitabine/Tenofovir Disoproxil Fumarate (EFV/FTC/TDF; Atripla): FDA label | Patient info
- Efavirenz/Lamivudine/Tenofovir Disoproxil Fumarate (EFV/3TC/TDF; Symfi, Symfi Lo): FDA label | Patient info
- Elvitegravir/Cobicistat/Emtricitabine/Tenofovir Alafenamide Fumarate (EVG/COBI/FTC/TAF; Genvoya): FDA label | Patient info
- Elvitegravir/Cobicistat/Emtricitabine/Tenofovir Disoproxil Fumarate (EVG/COBI/FTC/TDF; Stribild): FDA label | Patient info
- Emtricitabine/Rilpivirine/Tenofovir Alafenamide Fumarate (FTC/RPV/TAF; Odefsy): FDA label | Patient info
- Emtricitabine/Rilpivirine/Tenofovir Disoproxil Fumarate (FTC/RPV/TDF; Complera): FDA label | Patient info
- Emtricitabine/Tenofovir Alafenamide Fumarate (FTC/TAF; Descovy): FDA label | Patient info
- Emtricitabine/Tenofovir Disoproxil Fumarate (FTC/TDF; Truvada): FDA label | Patient info
- Lamivudine/Tenofovir Disoproxil Fumarate (3TC/TDF; Cimduo): FDA label | Patient info
- Lamivudine/Zidovudine (3TC/ZDV; Combivir): FDA label | Patient info
- Lopinavir/Ritonavir (LPV/r; Kaletra): FDA label | Patient info
Last updated on January 10, 2024